Systems Medicine: A Comprehensive Guide To Data Driven Personalised Healthcare

Systems medicine represents a revolutionary shift in how we approach health and disease. Unlike traditional medicine that often treats isolated symptoms, systems medicine takes a holistic view of the human body as an integrated system. It combines cutting-edge technologies like genomics, wearable devices, and artificial intelligence to understand how genes, environment, and our lifestyles interact and influence our health. I feel this new approach promises to transform healthcare from reactive to proactive, focusing on preventing disease before it occurs and personalising treatments to each individual's unique biological makeup. In this post I want to explore how systems medicine could fundamentally change our approach to healthcare in the coming years.
What is systems medicine?
Systems medicine represents a fundamentally new approach to healthcare that goes beyond traditional medicine's focus on isolated symptoms or diseases. It's the medical application of systems biology - the biological study of the complex interaction of systems rather than individual parts.
Traditional medicine has often been described as "reductionist," meaning it breaks down the body into smaller components and treats specific problems in isolation. For example, if you have heart disease, a cardiologist treats your heart; if you have digestive issues, a gastroenterologist treats your gut. While this approach has been successful in many ways, it doesn't always capture how these systems interact.
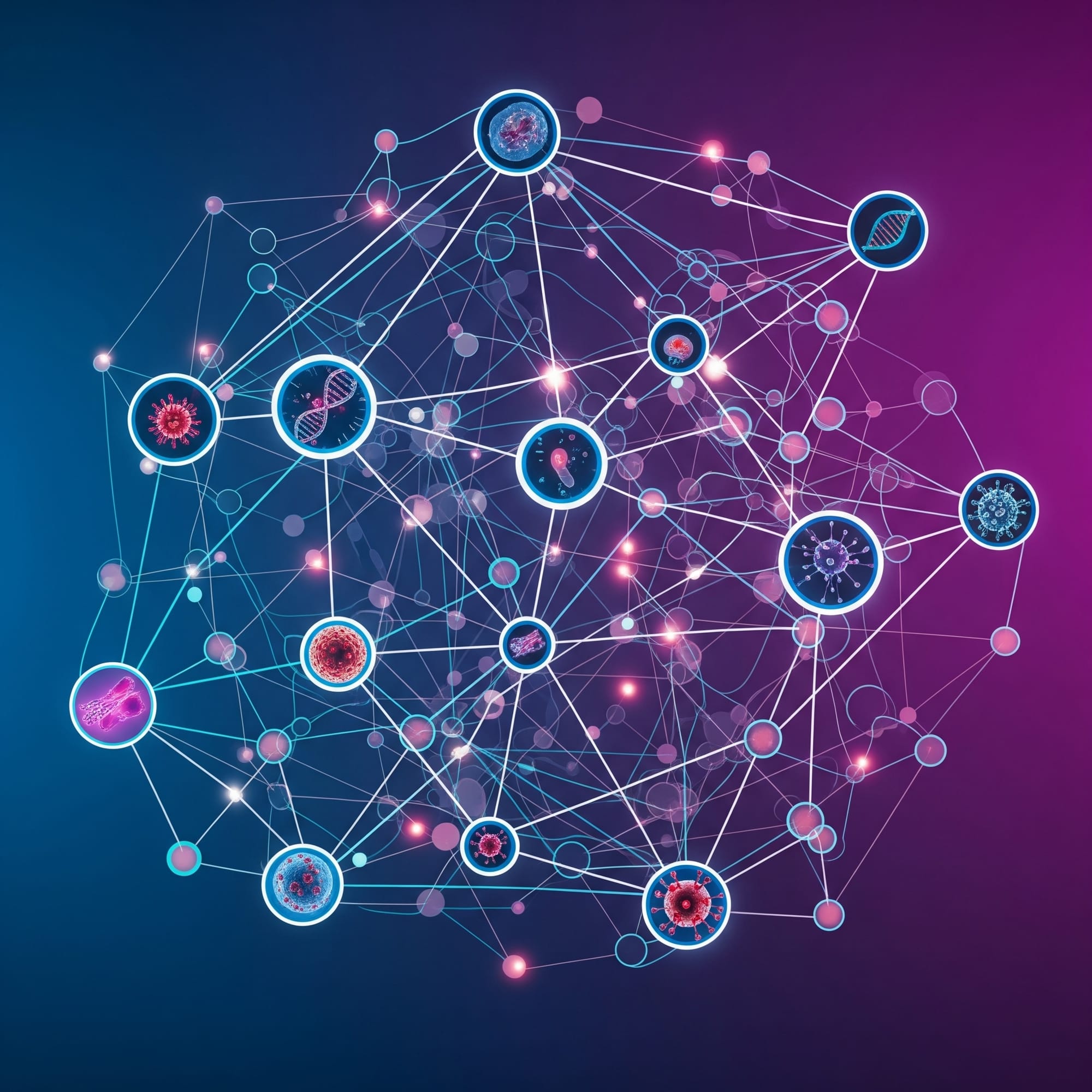
Systems medicine, by contrast, is "holistic" - it looks at your entire body as an interconnected network of networks. Through this approach multiple levels and their interactions with each other are considered:
- Molecular (genes, proteins, metabolites)
- Cellular (how cells function and communicate)
- Organ (how organs work together)
- Whole body (your overall physiology)
- Environmental (how lifestyle, diet, and environmental factors affect you)
What makes systems medicine different is that it integrates massive amounts of data from all these levels to get a complete picture of your health.
This isn't just about treating disease differently - it's about fundamentally redefining how we understand health itself. Systems medicine views health not as the absence of disease but as a dynamic state that emerges from properly functioning biological networks. When these networks become disrupted or imbalanced, disease can develop. By monitoring these networks over time, systems medicine aims to detect disruptions early, before symptoms appear, allowing for preventive intervention.
In essence, systems medicine sees each person as unique, with their own complex biological story. Rather than fitting patients into standardised disease categories, it aims to provide truly personalised healthcare based on your individual biological makeup and life circumstances.
Why Do We Need a Systems Medicine Approach to Health?
The True Complexity of Human Biology
Traditional medicine often looks at the body as a collection of separate parts, but the reality is far more interconnected. Our health emerges from dynamic interactions between multiple biological networks operating at different levels.
These networks exist at the molecular level (genes, proteins, metabolites), cellular level, organ level, and even extend to our interactions with the environment. Our biology resembles a dynamic network of networks. Disease doesn't just happen in isolation—it results from disruptions across these interconnected networks.
The traditional medical approach, a "one disease, one risk factor, one target" model, simply cannot capture this level of complexity. That is why I believe we need a more comprehensive approach that considers how the whole system functions together.
The Technological Revolution Making Systems Medicine Possible
We have seen a stratospheric rise in the collection of biomedical data over recent years. We can sequence a human genome for less than $1000. Wearable devices continuously track our vital signs and activities. Advanced functional imaging techniques provide detailed insights in to processes within our body. Blood tests can measure thousands of parameters simultaneously.
No doctor or scientist, no matter how brilliant, could possibly integrate and interpret all this information manually. To be meaningful, data must be analysed and converted into information and ultimately health knowledge.
This is where the technological foundation of systems medicine becomes essential. Advanced computational approaches like artificial intelligence and machine learning can identify patterns in these massive datasets that would be impossible for humans to detect. This helps make sense of the complex relationships between different biological components.
By embracing both the biological complexity of human health and the technological tools needed to understand it, systems medicine offers a fundamentally different approach to healthcare—one that aligns with how our bodies actually function as integrated systems rather than collections of separate parts.

How Does Systems Medicine Work?
The Integration of Multi-Dimensional Data
At its core, systems medicine works by gathering, connecting, and analysing diverse types of health-related data to create a complete picture of your health. Unlike traditional medicine that might focus on a single measurement or test result, systems medicine aims to collect what scientists call "holistic measurements"—data that are as comprehensive as possible.
These measurements span multiple dimensions and can include:
- Genomics: Your complete genetic makeup, which can reveal disease risk factors and how you might respond to medications
- Proteomics: The proteins circulating in your blood, which can indicate the state of your organs and tissues
- Metabolomics: Small molecules in your body that reflect your metabolism and nutrition
- Microbiome: The bacteria living in your gut and on your skin that influence many health processes
- Medical imaging: Advanced visualisation of your organs and tissues
- Electronic health records: Your medical history and previous test results
- Wearable devices: Continuous monitoring of heart rate, sleep patterns, activity levels, and more
- Lifestyle data: Information about diet, exercise, stress, and environmental exposures
We can think of this like a 'dynamic data cloud' giving a representation of life with billions of data points. This comprehensive approach allows systems medicine to capture the full complexity of your health in ways that isolated tests cannot.
From Data to Actionable Insights
The integrated data needs to be transformed into practical health insights. Systems medicine looks to do this by comparing your personal data patterns against comprehensive reference models of health and disease.
Systems medicine aims to provide actionable understandings of disease and wellness as a continuum of network states, unique in time and space to each individual human being.
Rather than simply classifying you as "healthy" or "sick," it can identify subtle transitions toward disease long before symptoms develop.
Through continuous monitoring, systems medicine looks to identify a "health trajectory"—the path your health is following over time. By detecting subtle, early deviations from your optimal trajectory, we could suggest personalised interventions to help you maintain or restore optimal health.
This approach transforms healthcare from reactive (treating disease after it develops) to proactive (maintaining health and preventing disease before it starts).

What Could Systems Medicine Mean for You?
Systems medicine is often described as "4P medicine" because it promises to transform healthcare in four fundamental ways: making it Predictive, Preventive, Personalised, and Participatory. Let's explore what each of these aspects could mean for your health.
Predictive: Insights To Your Health Risks
Traditional medicine typically responds to symptoms after they appear. We currently use excellent screening programmes which help us to identify individuals who may be at higher risks for certain conditions. Systems medicine offers an alternative approach by analysing comprehensive health data to predict disease before symptoms develop.
Recent exciting advancements in predictive medicine include in neurological disorders using digital biomarkers. Researchers have developed AI systems that can detect early signs of Parkinson's disease from subtle changes in voice patterns, with accuracy rates exceeding 95%. Similarly, MIT researchers found that machine learning algorithms analysing mouse movements could identify early motor impairments in Alzheimer's disease with 91% accuracy. These digital biomarkers offer non-invasive ways to monitor neurological health continuously.
In practice, this means you could receive early warnings about health risks specific to your biology, allowing for intervention long before conventional tests would detect a problem.
Preventive: Stopping Disease Before It Starts
Once potential health risks are identified, systems medicine shifts the focus from treating disease to preventing it entirely. This represents a radical departure from our current healthcare model, which primarily reacts to established disease.
The aim is to identify when your biological networks begin transitioning from healthy to disease states. By understanding these transitions at a systems level, precise interventions can be designed to restore normal network function before irreversible damage occurs.
With this technology, prevention can become highly personalised. Rather than following general health advice designed for the average person, you could receive precisely targeted recommendations based on your unique biology. These might include specific dietary changes, particular types of physical activity, personalised stress management techniques, or preventive medications—all selected because they address your specific biological vulnerabilities.
The European "Roadmap to Systems Medicine" emphasises that these preventive strategies would be continuously refined as new data is gathered about your health, creating an adaptive approach to disease prevention that evolves as your body changes over time.
Personalised: Tailored to Your Unique Biology
Systems medicine recognises that each person's biology is unique—what works for one person may not work for another with the same diagnosis. This understanding drives a move toward truly personalised healthcare.
By integrating your genomic data with other biological information, systems medicine can determine how you personally might respond to different treatments. For example, researchers have developed personalised medicine approaches that predict individual drug responses based on comprehensive molecular profiling.
This personalisation extends beyond medication to all aspects of health management. Your nutrition plan could be customised based on how your metabolism responds to different foods. Your exercise recommendations might be tailored to your specific cardiovascular and muscular biology. Even your sleep recommendations could be personalised based on your unique circadian rhythm patterns.
Participatory: You Become an Active Partner in Your Health
Perhaps the most transformative aspect of systems medicine is how it changes your role in healthcare. Rather than being a passive recipient of medical advice, you become an active participant in managing your health.
The technology-enabled nature of systems medicine allows you to continuously monitor aspects of your health and receive feedback about how your choices affect your biological systems. Wearable devices, home testing kits, and smartphone apps provide data that feeds into your personalised health model.
This participatory approach empowers you with knowledge about your own body that was previously unavailable. As a result, you can make more informed decisions about your health and work collaboratively with healthcare providers rather than simply following general health advice.
By combining these four elements—prediction, prevention, personalisation, and participation—systems medicine offers a fundamentally different approach to healthcare that puts you at the centre of your health journey.
When Will Systems Medicine Become Mainstream?
We have entered an era of rapid evolution in technology which will change many aspects of our lives. The previously impossible task of making sense of vast amounts of biological data is becoming feasible through advances in artificial intelligence, machine learning, and computational power.
This technological revolution is being recognised at the highest levels of UK healthcare policy. In September 2024, Health Secretary Wes Streeting outlined his vision for NHS reform at the Labour Party Conference, specifically noting how advances in data and genomics will enable healthcare to become "more predictive, more preventative, and more personalised than ever before." This vision directly aligns with the core principles of systems medicine.
Several concrete initiatives are already translating these aspirations into reality:
Our Future Health - Launched in 2022, Our Future Health is the UK's largest health research program, aiming to collect detailed health data from 5 million volunteers. As of October 2024, over 1 million people have already enrolled. The program combines genetic information with clinical, lifestyle, and environmental data to develop more precise approaches to disease prevention and early detection. This large-scale integration of multi-dimensional health data exemplifies systems medicine principles in action.
NHS Genomic Medicine Service - Since its nationwide implementation in 2018, the NHS Genomic Medicine Service has been bringing genomic testing into mainstream healthcare. Building on the success of the 100,000 Genomes Project, the service now offers whole genome sequencing as standard care for patients with certain rare diseases and cancers. This integration of genomic information with traditional clinical care represents an important step toward the comprehensive, multi-level approach that defines systems medicine.
My vision of how systems medicine will develop is with initial breakthrough developments in certain medical fields. These will then coalesce to form a more generalised, holistic healthcare model that treats people as complete individuals rather than collections of separate symptoms or diseases. Patients will become increasingly empowered, interested and excited to gain deeper insights and ownership of their health through access to their own comprehensive data. We will be more aware and connected with our health - seeing the impacts and improvements of decisions we make day to day. My hope would be that this leads to better health decisions and lifestyle choices leading to healthier, happier communities.
What Challenges Need to Be Overcome?
While systems medicine offers tremendous potential, it all poses a number of challenges and questions that I feel are important to address. These will need continuous, careful consideration when looking at implementing systems medicine approaches. Some of these topics include:
Data Processing and scientific review As discussed earlier, systems medicine generates unprecedented volumes of complex biological data. While technology is rapidly evolving to handle this complexity, we still need robust, longitudinal studies to validate these approaches and assess outcomes in the real world. New computational methods using artificial intelligence and machine learning show promise, but require careful testing to ensure that identifying patterns and the resulting interventions actually lead to better health outcomes and do not cause harm.
Data Privacy and Protection The comprehensive health profiles created through systems medicine contain our most intimate biological information. Protecting this data is paramount, especially as commercial interests seek access to valuable health information. Questions remain about who owns this data, how consent is managed over time, and how to prevent unauthorised use or sale of personal health information.
Risk of Over-Medicalisation As noted in research on systems medicine, there's a risk of what some researchers call "holistic medicalisation" – where each person's entire life process becomes defined in biomedical terms and subjected to continuous monitoring and control. When every biological variation becomes potentially "actionable," we risk turning normal human diversity into medical conditions requiring intervention. Finding the right balance between beneficial early intervention and unnecessary treatment will be crucial. I found this paper on 'O4 medicine' (overtesting, overdiagnosis, overtreatment, overcharging) particularly insightful and useful in considering the pitfalls of a 4p medicine approach.
Transforming Healthcare Delivery Systems Our current healthcare systems are designed around episodic care for established diseases, not continuous health monitoring and early intervention. Implementing systems medicine requires fundamentally new ways of working – from how medical professionals are trained to how care is organised and delivered.
Ensuring Equity Across Diverse Populations Advanced technologies often reach privileged populations first, potentially widening existing health inequalities. Systems medicine must be developed and implemented with explicit attention to diversity and inclusion. This means ensuring that baseline data represents all populations and that the benefits of these new approaches reach everyone, not just those with resources and healthcare access.
Addressing these challenges requires collaboration between scientists, healthcare providers, policymakers, ethicists, and patients. With thoughtful implementation that proactively tackles these issues, systems medicine can fulfil its promise of transforming healthcare while avoiding potential pitfalls.
What are your thoughts? Please add any ideas or comments in the section below
Conclusion: A New Era of Healthcare
The healthcare landscape of tomorrow looks dramatically different from what we know today. Systems medicine represents not just an incremental improvement to our current approaches, but a fundamental reimagining of how we understand and manage health.
Imagine a future where you're deeply connected to your own health data—not just occasional snapshots from yearly checkups, but a continuous, comprehensive understanding of your unique biology and its patterns. Rather than receiving generic recommendations based on population averages, your healthcare becomes truly personalised, tailored to your specific genetic makeup, environmental exposures, lifestyle choices, and current biological state.
This vision aligns perfectly with what researchers call "4P medicine"—healthcare that is Predictive, Preventive, Personalised, and Participatory. Systems medicine enables all four of these dimensions.
This transformation represents a profound shift in focus from simply extending life span to maximising health span—the number of years we live in good health, free from debilitating disease. Rather than just adding years to life, systems medicine aims to add life to those years. It prioritises quality of life alongside longevity, recognising that our goal isn't merely to live longer, but to thrive throughout our lives.
The road to this future contains challenges, but the potential benefits are profound. Systems medicine promises not just longer lives, but fundamentally healthier ones—with more years spent in wellness rather than managing chronic conditions. It offers the possibility of healthcare that works with our bodies' natural systems rather than intervening only when those systems fail.
As this new paradigm unfolds, we all have an opportunity to engage with and shape its development. The future of healthcare isn't just something that happens to us—it's something we create together, combining the best of technological advancement with our deeply human desire for health and wellbeing throughout our entire lives.
References
- Apweiler, R., Beissbarth, T., Berthold, M. R., Blüthgen, N., Burmeister, Y., Dammann, O., ... & Wolkenhauer, O. (2018). Whither systems medicine?. Experimental & Molecular Medicine, 50(3), e453. https://doi.org/10.1038/emm.2017.290
- Auffray, C., Chen, Z., & Hood, L. (2009). Systems medicine: the future of medical genomics and healthcare. Genome Medicine, 1(1), 2. https://doi.org/10.1186/gm2
- Lemmen, C., Woopen, C., & Stock, S. (2021). Systems medicine 2030: A Delphi study on implementation in the German healthcare system. Health Policy, 125(1), 104-114. https://doi.org/10.1016/j.healthpol.2020.11.010
- Vogt, H., Hofmann, B., & Getz, L. (2016). The new holism: P4 systems medicine and the medicalization of health and life itself. Medicine, Health Care and Philosophy, 19(2), 307-323. https://doi.org/10.1007/s11019-016-9683-8
- Wang, H., Pujos-Guillot, E., Comte, B., de Miranda, J. L., Spiwok, V., Chorbev, I., ... & Zheng, H. (2021). Deep learning in systems medicine. Briefings in Bioinformatics, 22(2), 1543-1559. https://doi.org/10.1093/bib/bbaa237
- Wolkenhauer, O., Auffray, C., Jaster, R., Steinhoff, G., & Dammann, O. (2013). The road from systems biology to systems medicine. Pediatric Research, 73(4), 502-507. https://doi.org/10.1038/pr.2013.4
- Yurkovich, J. T., Evans, S. J., Rappaport, N., Boore, J. L., Lovejoy, J. C., Price, N. D., & Hood, L. E. (2023). The transition from genomics to phenomics in personalized population health. Nature Reviews Genetics. https://doi.org/10.1038/s41576-023-00674-x
- Gündüz H. (2019). "Deep learning-based Parkinson's disease classification using vocal feature sets." IEEE Access, 7:115540-115551.
- Seelye A, et al. (2015). "Computer mouse movement patterns: A potential marker of mild cognitive impairment." Alzheimer's & Dementia: Diagnosis, Assessment & Disease Monitoring, 1(4):472-480.